Falls in the home are a common concern, especially for older adults, and can result from poor balance, muscle weakness, foot pain, or environmental hazards. Cluttered walkways, loose rugs, and slippery bathroom surfaces often increase the risk of injury. Preventing falls begins with keeping living spaces clear and well organized, installing grab bars in the bathroom for added stability, using slip resistant bath mats, and refraining from using a ladder without proper support. Wearing supportive footwear indoors can also improve balance. A podiatrist can assess foot health, address pain or instability, and recommend supportive devices to enhance safety. If you have injured your foot or ankle from falling, it is suggested that you consult a podiatrist who can treat various foot conditions, and guide you on additional fall prevention techniques.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Pedram Aslmand, DPM from Advanced Foot and Ankle Center. Our podiatrist will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
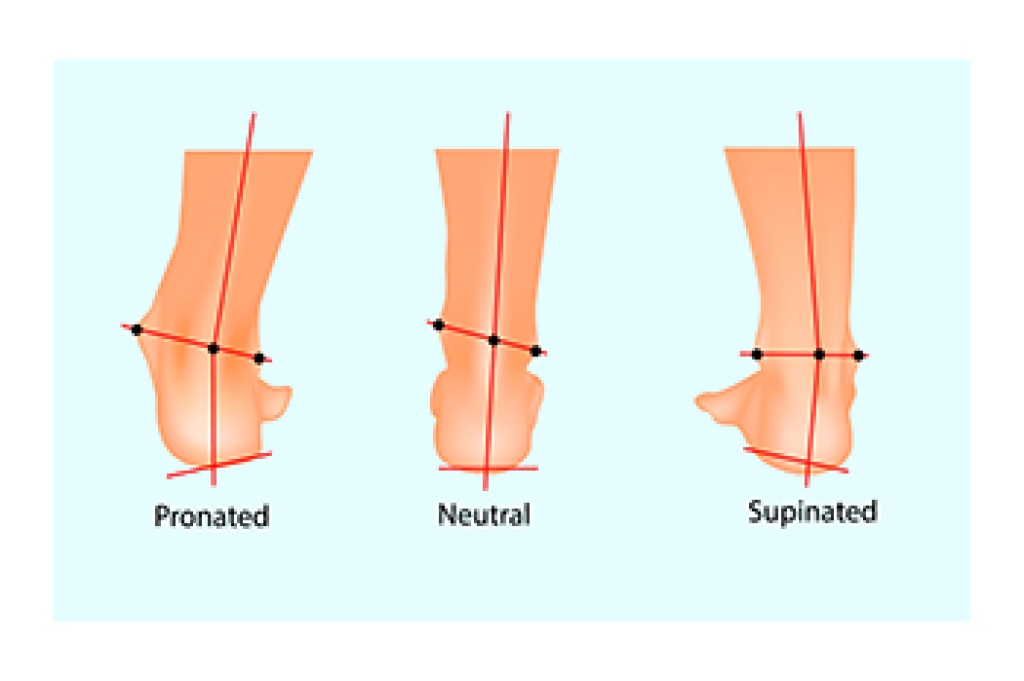
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our offices located in Long Beach, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.